M.E./CFS Treatment in London and Online
Fatigue conditions, such as Myalgic Encephalomyelitis (M.E.)/Chronic Fatigue Syndrome (CFS) and Fibromyalgia, can be debilitating conditions and have the potential to take over people’s lives. If you have these conditions, at Therapy Central we can offer expert support with therapists who specialise in fatigue conditions to help you to find ways to manage your symptoms to gain relief from them and to get back doing more of what you used to. Get in touch today for M.E. and Chronic Fatigue treatment in London or Online here.
Work with our qualified M.E./CFS Treatment therapists today.
Request a free 15min consultation

Discover M.E./CFS Treatment
CFS: Chronic Fatigue Syndrome
It is key to look after yourself when you have M.E./CFS. Your body is working harder to just function and for this reason it is difficult to do as much as you used to. If you had another physical health condition, such as arthritis or cardiac problems, you would be listening to your body and looking after yourself. The same should be the case with M.E./CFS. The two CFS treatment that we offer at Therapy Central, Energy Management and Psychological Therapy, can help you to do just that. They can help you to look after your wellbeing better in order to give you the best chance of working towards recovery.
Unfortunately at the moment there is not a medical cure for M.E./CFS. It seems that the bodily systems underlying M.E./CFS is complex and the symptoms affect various aspects of an individual’s life. Therefore, an approach is needed to tackle M.E./CFS from different angles which is something that our Fatigue Specialists can provide at Therapy Central.
What is M.E./CFS?
M.E/CFS is a physical health difficulty. It can be difficult to understand, even for those suffering from it partly due to its complex and unpredictable nature; symptoms can fluctuate for no apparent reason. M.E./CFS can range from mild to severe. It can affect every system in the body and involve a constellation of symptoms which can include:
- Extreme tiredness
- Flu-like symptoms
- Brain fog
- Widespread pain
- Post-exertional malaise
- Recurrent sore throat/swollen glands
- Poor temperature control
- Difficulties sleeping, unrefreshed sleep
- Digestive problems
- Intolerances to foods, medication, light, sound, touch
- Dizziness
- Cognitive difficulties: poor memory, concentration, attention
If you have M.E./CFS you may experience some or all of these symptoms. This is not an exhaustive list of symptoms so there may be other symptoms that you experience.
There has been a large debate about whether M.E. and CFS are distinct. Additionally, other terms have been used to describe M.E/CFS, such as:
- Post-viral fatigue syndrome (PVFS)
- Post-exertional malaise
- Chronic fatigue immune dysfunction syndrome (CFIDS)
Many people, such as health professionals within the NHS, use the terms M.E. and CFS interchangeably because of the large overlap in symptoms. Therefore, M.E./CFS will be the term used here. Fibromyalgia is another fatigue condition which shares lots of similarities with M.E./CFS. Much of what is to be discussed below is also relevant if you are struggling with fibromyalgia.
What Causes M.E./CFS?
Research and experience suggest that various factors play a role in the development and maintenance of M.E./CFS. It may be that all of these factors resonate with you or just some.
Vulnerability Factors
Below is an outline of factors that people with M.E./CFS often experience. These factors are considered to put an extra strain on the body and brain which may lead people to being vulnerable to developing this condition later in life.
Virus
Research suggests that 30% of people who have glandular fever (caused by the Epstein-Barr virus) develop M.E./CFS. This suggests that viruses play a causal role. Individuals may have had glandular fever several years prior to the development of M.E./CFS. They may not have even known they had glandular fever in the past. Blood tests can detect whether one has certain antibodies which indicate they have had glandular fever in the past.
Personality Traits
There are common personality traits that are seen in people with M.E./CFS. We know that resting the mind and body is needed for restoration and to re-energise. However, a large proportion of people with M.E./CFS have certain personality traits which contribute to significant strain on their brain and bodies coupled with little rest.
For example, many people with M.E./CFS are perfectionists; they work to high standards in various areas of their lives. This tends to lead them to push themselves, have little rest and experience heightened stress levels partly due to the pressure they place on themselves.
Another trait that is often seen in those with M.E./CFS is doing lots for others. This can be at the expense of their own needs, such as giving themselves little down time. Sometimes the pressure to please others can be stressful and it can foster resentment.
Triggering Factors
Below are the common factors that people experience before the onset of M.E./CFS which are thought to add further strain on the brain and body which contributes to M.E./CFS being triggered.
Surgery/Virus
Some people may have had some form of surgery and/or experienced a virus or several viruses prior to the onset of M.E./CFS. Both of these put a strain on the immune system.
High Stress Levels
Around the onset of M.E./CFS people often experience high stress levels. This could be due to one particularly stressful event or an accumulation of stressful events where the brain and body were working hard with insufficient rest. This may include a high work load at work or school or at home. Or perhaps there were relationship difficulties. The high stress levels may have even been associated with a life event that would usually be deemed positive, such as moving house and getting married.
It is really important to note here that because stress levels are being mentioned it does not mean for one second that it is being suggested that M.E./CFS is all in a person’s head (which is a message people with M.E./CFS often receive from others). Physical symptoms in M.E./CFS are very much real and have a physiological basis. It is believed that stress is likely to trigger M.E./CFS in many people via the impact it has upon the brain and body; it puts an extra strain on them which then leads to physiological changes resulting in M.E./CFS.
Can these Triggering Factors Lead to the Onset of M.E./CFS?
As noted above, preceding the onset of M.E./CFS there appears to be a significant amount of demand on the brain and body whether this is due to things such as a virus, over-exertion, stress and having insufficient rest or any combination of these. During these times our bodily systems work hard for the brain and body to function well and meet these demands as well as protect the brain and body in the meantime. These systems can be likened to an electrical system. In an electrical system when there is a large surge in electricity the fuse blows to protect the system. In a similar way, if there is a large surge of demand placed upon the brain and body, changes occur in the body and fatigue results as a form of protection; fatigue forces you to stop and slow down.
Physiology Underlying M.E./CFS
Unfortunately M.E./CFS has been a neglected field when it comes to research into the physiology underlying it. Thankfully, it seems that gradually more research is being conducted into it, but arguably, still not enough! Research suggests that there is dysregulation in bodily systems including the immune system, the autonomic nervous system, the endocrine system, the gastrointestinal system, the cardiovascular system, the muscular system and the hypothalamus-pituitary-adrenal axis (HPA-axis). Also, a leading theory into the cause of M.E./CFS is a dysfunction with mitochondria which is the part of cells responsible for generating energy. Additionally, the role of genes and how they function are thought to play a role.
It can be overwhelming and confusing to understand all of the emerging theories and research when different parts of the body are thought to play a role. It is likely that the physiology underlying M.E./CFS is highly complex as many bodily systems are involved and are likely to interact with each other.
Common Struggles Faced by People with M.E./CFS
These are common struggles that people with M.E./CFS face. It may be that you resonate with all of these struggles or maybe just some.
Others’ Lack of Understanding
Hopefully you will have some good support around you. However, very often people with M.E./CFS come across friends, family and/or medical professionals who demonstrate a lack of understanding of their condition. To make matters worse, you may have received negative judgments and been told that others do not believe that the condition exists altogether, suggesting “it’s all in your head”. You may find yourself trying to explain the condition frequently to others to help them understand, but your attempts may be futile. Or you may have given up trying to explain it altogether. It may have taken years to receive a diagnosis which may have partly arrived due to the process of eliminating other causes. However, it may also be due to medical professionals lacking knowledge of M.E./CFS and even attributing the symptoms to depression and/or anxiety.
Not Being Able to Do What I Used to
The symptoms of M.E./CFS can unfortunately lead to a loss of routine and role(s). Some people reduce or stop working, socialise less or not at all and reduce or stop engaging in hobbies. This is understandable given how individuals feel physically. It is often hard facing the fact that one is not able to do as much as they used to and fulfil certain roles to the degree that they did before they developed M.E./CFS. Life has perhaps become increasingly narrow and limited to doing things that they have to do as opposed to what they want to do. You may have had to make adjustments to things that you do. It makes it especially hard if you were previously an active and productive person, which is often the case in those with M.E./CFS. At times you may find yourself not wanting to give in to the condition and so push yourself to do the things you used to and to the extent you used to. However, this often exacerbates symptoms, either immediately or the exacerbation in symptoms can have a delayed onset.
Its Unpredictable Nature
M.E./CFS symptoms often fluctuate. When the symptoms flare up the triggers can be clear, such as over-exertion (even though this amount of exertion may have been considered a small amount before the onset of M.E./CFS) and a virus (cold/flu). However, at other times when there is a flare up, there is no known trigger. To confuse things more, there are times when a certain amount of activity triggers the symptoms but at other times the same amount of activity does not trigger the symptoms. This can make you feel less in control of your M.E./CFS, it can make it difficult to work out approximately what amount of activity is tolerable without exacerbating your symptoms and can generally add to your frustrations around your condition.
It can be a Scary Condition
The vast array of unpleasant symptoms and the fact that they can be severe at times (or much of the time for some people) can make it a scary condition to experience. Even after going through a battery of investigations which have ruled anything more sinister out many people with M.E./CFS are fearful that there is an underlying cause apart from the M.E./CFS that has yet to be identified. This may result in you wishing to be further investigated and, funds permitting, you may have found yourself paying for such investigations privately. Another aspect of the condition that can be scary is that even if your symptoms improve slightly following a period of severe symptoms, you may remain highly fearful of doing things that may lead to another exacerbation of your symptoms.
I’ve Tried Lots of Different Therapies
Given people’s determination to be rid of their symptoms, very understandably, many people with M.E./CFS have tried various types of therapy, including reiki, B12 injections, vitamins, hypnotherapy, aromatherapy, acupuncture, nutritional advice, massage, naturopath and reflexology. You may have seen some benefits, which may have been short-lived, or perhaps no benefits at all. It may be that a lot of time, energy and money have gone into these therapies. Altogether, this has perhaps left you feeling even more frustrated and exasperated.
M.E./CFS Treatment
Energy Management
Pacing and Promoting Energy
In Energy Management, you will work with your Fatigue Specialist to manage all aspects of the physical side of your health and wellbeing. In the early stages of Energy Management, your therapist will help to build upon your existing knowledge of the biological systems impacting on your day-to-day symptoms, life and function. Having an in-depth understanding of the possible reasons symptoms behave as they do and where they come from can reduce the distress caused by them and provide further insights into their management.
You will be helped to fine tune ways of making everyday tasks more manageable; the “have to be done” list can often be long and may drain a lot of energy. However, there are many options available to us to strike a balance between getting things done without making symptoms much worse or having no energy left for anything else.
Equally, if not more importantly, you will be supported to develop methods that allow safe re-introduction of your “want to do” list: activities that you enjoyed and loved. Those things that helped you unwind or relax, helped you feel fulfilled or gave you a sense of achievement and wellbeing. This can help to improve your quality of life.
Topics that are often covered in Energy Management are; sleep; how aspects of diet and nutrition can influence symptoms; addressing issues such as back or neck pain or other physical factors that limit you; pacing energy at work, home and socially; safe approaches to many different kinds of exercise and relaxation techniques. However this list is not exhaustive and each person’s management plan is tailored to them.
Psychological therapy
In the early stages of therapy, you will be helped to gain an in-depth understanding of how your M.E./CFS developed and is maintained. You will work together with your Fatigue Specialist Psychologist to build upon your understanding of the physiology underlying M.E./CFS. This guides the therapy in terms of what aspects should be focused on in order to work towards recovery.
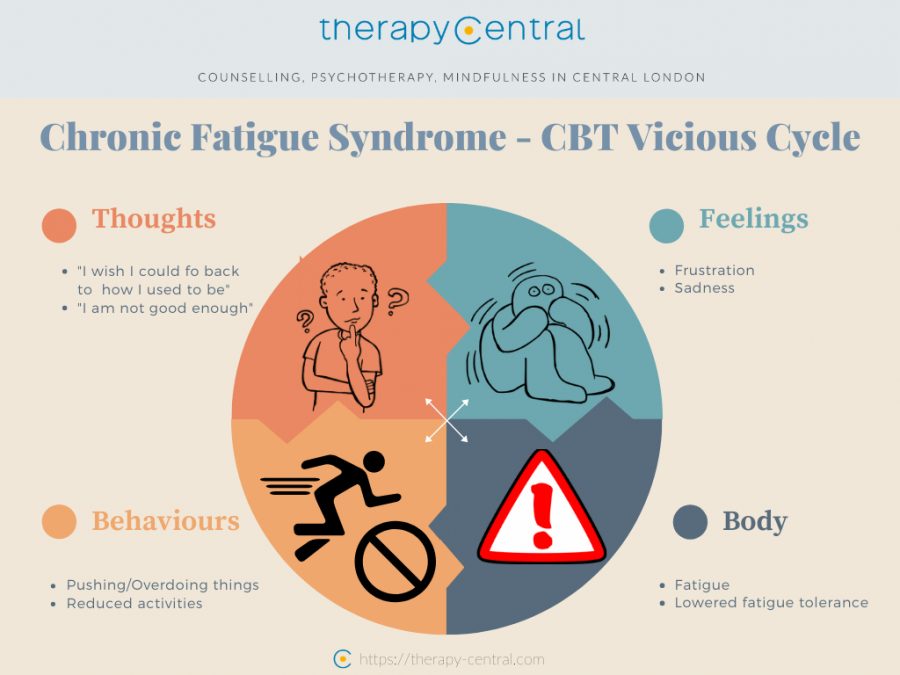
You will be introduced to various practical and psychological (meaning ways to address thoughts, emotions and behavioural patterns) coping strategies to better manage your symptoms which have all been supported by solid research. Additionally, some people can find it helpful to use the therapeutic space to explore and process the impact of the M.E./CFS and the numerous challenges they have faced in a warm, supportive and non-judgmental environment. The overall aim is to work collaboratively with your therapist to find ways to improve your physical and emotional wellbeing which will have a positive influence upon the bodily systems that underlie M.E./CFS. This can help to reduce symptoms and improve quality of life. Therapy will be individualised to suit your needs. See below an example of a CBT based vicious cycle of CFS.
What are the Benefits of M.E./CFS Treatment?
Research shows that activity management and pacing that Energy Management entails as well as Psychological Therapy can benefit many people with M.E./CFS. Hundreds of people with M.E./CFS that we have provided therapy to have reported various significant improvements. Measures that are completed before and after therapy with individuals with M.E./CFS supports this. Improvements are often seen in the following areas:
- Reduction in M.E./CFS symptoms, such as fatigue, pain and brain fog
- Increased energy
- Improved physical functioning
- Improved quality of life
- Socialising more
- Increased activity levels
- Increased confidence in ability to manage symptoms
- Improved emotional wellbeing
- Prevention of deterioration in physical and emotional wellbeing as well as functioning
How Long Does M.E./CFS Treatment Last?
Some people can make good improvements in up to around ten sessions of Energy Management or Psychological Therapy. However, sometimes it is helpful for therapy to extend beyond ten sessions and to have up to around fourteen sessions in total for several reasons; 1) It can take time for the bodily systems that underlie M.E./CFS to respond to the good changes you make in therapy and 2) There are numerous ways to try to manage M.E./CFS that you will be introduced to which can take time and it is not in your best interests for this to be rushed. It can be helpful to have both Energy Management and Psychological Therapy, receiving one after the other is completed.
What M.E./CFS Treatment is Right for Me: Energy Management or Psychological Therapy?
Some people choose to receive just Energy Management or Psychological Therapy or both, receiving one after the other. Whether you choose to pursue Energy Management or Psychological Therapy first is dependent upon what you wish to mainly focus on. Both take a holistic approach, however, the focus of Energy Management is tilted towards learning practical and physical tools to manage your condition. Psychological Therapy also involves helping you to learn practical tools as well as psychological tools to manage your condition. Compared to Energy Management, Psychological Therapy has more of an emphasis on helping to improve your emotional wellbeing. If you are struggling to decide which therapy to pursue first we can offer a free 15 minutes telephone consultation to help you make a decision.
Our therapists specialised in M.E./CFS Treatment
All of our therapists are qualified psychologists, psychotherapists or counsellors registered with several professional bodies. These include the Health and Care Professions Council (HCPC), the British Psychological Society (BPS), as well as, BACP, UKCP and BABCP.
Our therapists use CBT therapy, psychodynamic, humanistic and integrative approaches tailored around your needs to help you deal with your unique challenges and reach your goals.




Testimonials
⭐⭐⭐⭐⭐
The Therapist l had was absolutely brilliant with me. He had patience with me and bit by bit l gained a little of confidence to try and get out and go on the buses.
He deserves an award and if l could l would in the beginning l thought how is this person going to get me back on public transport but he did he gave me the confidence l lost and now have back.
I will never forget him and what he has done for me. I wish him nothing but the best in his life.
(Patricia)
⭐⭐⭐⭐⭐
My therapist was excellent. I highly recommend her and I am truly thankful for my sessions, I left feeling confident and positive.
The mental tools, systems and approaches I have been able to develop with her and use in my life have been hugely beneficial.
Thank you to all at Therapy Central.
(John)
⭐⭐⭐⭐⭐
The Therapist really gave me the space to talk and express my feelings and fears in a very comforting environment.
She was there not only to listen, but challenge my thinking, guide me during the uncertainty I was experiencing and give me useful and practical tips to improve my mental health and wellbeing. Highly recommended!
(George)
⭐⭐⭐⭐⭐
Working with the therapist has been a life-changing experience. Each session has been invaluable, helping me gain a good understanding of CBT methodology enabling me to incorporate ways to combat stress and anxiety in my daily life.
The Therapist shows that she really cares and has the ability to make you feel calm whilst discussing any personal issue.
(Richard)
Fees & Insurances
Therapy, Counselling and CBT sessions are 50 minutes long and are usually held at regular weekly time slots.
Free
15 Minute Initial
Phone Consultation
£80 - £125
Psychological Therapy/
Counselling (Self-funded)
£115 - £150
Couples Therapy/
Family Therapy
Covered by
Your Private Healthcare Insurance Provider
Our Physiotherapist specialised in M.E./CFS Treatment in London
Gina Wall, Musculoskeletal Physiotherapist. Pain and Fatigue Management Specialist, BSc Physiotherapy, MSc Pain Management
I have extensive experience of working with people with M.E./CFS, including managing a busy NHS Fatigue Service in London. For many years I have provided Energy Management to many people with M.E./CFS.
Working collaboratively with people living with M.E./CFS to help them manage their health has shown me first-hand the positive experiences that can come from being provided with information on the physiology of the condition.
My extensive background in musculoskeletal physiotherapy and pain and fatigue management enables me to assist you with managing all aspects of the physical side of your health and well-being.
It can be helpful to receive help to manage your chronic pain at any stage given that they can be highly challenging to experience both physically and emotionally. However, many people seek therapy when they feel relatively hopeless, when they have exhausted the medical route, when they are struggling to manage, they do not feel in control and it is having a large negative impact upon their lives. These are signs that certainly indicate that therapy can be helpful. It can also prove helpful to reach out for support in the earlier stages of your condition.
Gina Wall

M.E./CFS Treatment in London & Online
If you are looking for specialist Chronic Fatigue Treatment in London or online, including either Energy Management (with a physiotherapist) or psychological therapy, at Therapy Central we can help you learn the strategies you need to start managing your condition effectively and reducing its impact on all areas of life. As a result, you’ll be enabled to make the crucial changes to bring balance and fulfilment back into your life. No one should face M.E. or a chronic fatigue syndrome alone.
Get professional help with M.E./Chronic Fatigue in London and Online today. Contact us for a free 15 min consultation with a Chronic Fatigue Specialist to see if our help would fit your needs. You can also get in touch via email at info@therapy-central.com or call us at (+44) 020 348 82797.

FAQ
What happens after I make an enquiry?
After receiving your enquiry we’ll contact you to organise a FREE phone consultation. You will be able to tell us more about your specific circumstances and needs and ask any questions you have. Then, if you want to proceed with therapy or counselling, we’ll match you with the therapist(s) with the best expertise to help you with your challenges and send you a list of their available appointment slots. If you’re satisfied with one of these, we can then go ahead and book your first appointment. You can also request to work with a specific practitioner and, depending on availability we’ll try accomodate this.
What happens at my first appointment with the therapist?
Your first session will likely be different than future appointments. You and your therapist will get to know each other and will begin to build a working alliance. It will be a chance to have the confidential space to express your circumstances, feelings and thoughts and being listened to with depth, attention, empathy and without judgement . Your therapist will likely ask you more about your reasons for seeking therapy, and any symptoms you’re experiencing. You may also be asked questions about your past and the history of your issues, as well as how they currently impact your life in the present. Finally, your first session may be a powerful place to discuss what you would like to achieve with therapy and agree on the length, methods and approaches of treatment.
Is online therapy effective?
If you choose online over in-person therapy rest assured that this has been proven to be just as effective as regular face to face therapy, and in some cases even more effective. In addition, choosing online therapy brings additional benefits, for example avoiding longer waiting times, greater flexibility with appointments and you won’t need to travel to our practice. You can enjoy online therapy from the comfort of your home.
How long the Therapy/counselling sessions last?
Therapy/counselling sessions last 50 minutes and are held at regular weekly time slots. On occasions we are able to allow some flexibility. This can be discussed with your therapist.
Do you offer reduced rates/concessions?
We offer low-cost rates to people with a low income, unemployed or students. Please let us know in your enquiry if you would like a concession rate and how you qualify for this. Depending on the availability of our therapists, we’ll do our best to accommodate your request.
Do you have a cancellation policy?
We have a 48 hours no-fee cancellation policy. However you will be charged for sessions missed without giving the full notice.
Our Practice in Central London
Our comfortable and confidential therapy rooms are conveniently located 3 min walk from Oxford Circus station, in Central London (see map below). Change starts with Talking!
Authors:
Dr Amy Smith, Counselling Psychologist
Dr Raffaello Antonino, Counselling Psychologist
Learn more:
Other issues we work with at Therapy Central
NHS: Understanding Fatigue
NHS: Chronic Fatigue Syndrome info
References:
Esfandyaour, R. et al. (2019) A nanoelectronics-blood-based diagnostic biomarker for myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). Proceedings of the National Academy of Sciences, 116 (21), 10250-10257.
Research that supports the effectiveness and efficacy of Energy Management and Psychological Therapy for M.E./CFS:
Deale A, Husain K, Chalder T, Wessely S. Longterm outcome of cognitive behavior therapy versus relaxation therapy for chronic fatigue syndrome: a 5-year follow-up study. Am J Psychiatr. 2001;158:2038–2042. doi: 10.1176/appi.ajp.158.12.2038
Geraghty, K. et al. (2017). Myalgic Encephalomyelitis/Chronic Fatigue Syndrome patients’ reports of symptom changes following cognitive behavioural therapy, graded exercise therapy and pacing treatments: Analysis of a primary survey compared with secondary surveys. Journal of Health Psychology. 24, (10)
Jonsjo, M., Wicksell, R., Holmstrom, L., Andreasson, A. And Olsson, G. (2019). Acceptance & Commitment Therapy for ME/CFS (Chronic Fatigue Syndrome) – A feasibility study. Journal of Contextual Behavioral Science, 12, 89-97.
Price, J., Mitchelle, E. and Tidy, E. (2008). Cognitive behavior therapy for chronic fatigue syndrome in adults. Cochrane Database Syst Rev, 3. doi:10.1002/14651858.
Prins J, Bleijenberg G, Bazelmans E et al. Cognitive behaviour therapy for chronic fatigue syndrome: a multicentre randomised controlled trial. Lancet 2001; 357: 841–7.
Research into the Physiology Underlying M.E./CFS
de Vega, WC. (2018). DNA methylation modifications associated with Glucocorticoid sensitivity and clinical subtypes of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS). [Online] available at https://tspace.library.utoronto.ca/handle/1807/89701
Kempke, S. et al. ( 2016). Self-critical perfectionism predicts lower cortisol response to experimental stress in patients with chronic fatigue syndrome. Health Psychology, 35 (3)
German, A. et al. (2020). Comprehensive circulatory metabolomics in ME/CFS reveals disrupted metabolism of Acyl lipids and steroids. Metabolites, 10, (1)
Giloteaux, L. et al. (2016). Reduced diversity and altered composition of the gut microbiome in individuals with Myalgic Encephalomyelitis / Chronic Fatigue Syndrome. Microbiome. 4 (1)
Polli, A. et al. (2019). Exercise induced hyperalgesia, complement system and elastase activation in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome- a secondary analysis of experimental comparative studies. Official Journal of the Scandinavian Association for the study of Pain. 19, (1)
van Campen, LMC et al. (2020). Cerebral blood flow is reduced in ME/CFS during head-up tilt testing even in the absence of hypotension or tachycardia: A quantitative, controlled study using Doppler echography. Clinical Neurophysiology Practice, 5, 50-58
van Oosterwijck, J. et al. (2017). The role of autonomic function in exercise induced endogenous analgesia: a case-control study in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome and healthy people. Pain Physician, 20, (3)









